Doctor For SRS in Delhi NCR, Stereotactic Radiosurgery Hospital In India
Stereotactic radiosurgery (SRS) is a non-surgical radiation therapy used to treat functional abnormalities and small tumors of the brain. It can deliver precisely-targeted radiation in fewer high-dose treatments than traditional therapy, which can help preserve healthy tissue. When SRS is used to treat body tumors, it’s called stereotactic body radiotherapy (SBRT). SRS and SBRT are usually performed on an outpatient basis. Ask your doctor if you should plan to have someone drive you home afterward and whether you should refrain from eating or drinking or taking medication several hours before treatment. Tell your doctor if there’s a possibility you are pregnant or if you’re breastfeeding or if you’re taking oral medication or insulin to control diabetes. Discuss whether you have an implanted medical device, claustrophobia or allergies to contrast materials.
What is stereotactic radiosurgery and how is it used?
-
Stereotactic radiosurgery (SRS) is a highly precise form of radiation therapy initially developed to treat small brain tumors and functional abnormalities of the brain. The principles of cranial SRS, namely high precision radiation where delivery is accurate to within one to two millimeters, are now being applied to the treatment of body tumors with a procedure known as stereotactic body radiotherapy (SBRT).
Despite its name, SRS is a non-surgical procedure that delivers precisely-targeted radiation at much higher doses, in only a single or few treatments, as compared to traditional radiation therapy. This treatment is only possible due to the development of highly advanced radiation technologies that permit maximum dose delivery within the target while minimizing dose to the surrounding healthy tissue. The goal is to deliver doses that will destroy the tumor and achieve permanent local control.

Who will be involved in this procedure and who operates the equipment?
-
The treatment team is comprised of a number of specialized medical professionals, typically including a radiation oncologist, medical radiation physicist, radiologist, dosimetrist, radiation therapist, and radiation therapy nurse.
The radiation oncologist and, in some cases, a neurosurgeon lead the treatment team and oversee the treatment; they outline the target(s) to be treated, decide on the appropriate radiation dose, approve the treatment plan, and interpret the results of radiosurgical procedures.
A radiologist interprets imaging that identifies the target(s) to be treated in the brain or body.
The medical radiation physicist ensures the delivery of the precise dose of radiation.
The physicist, or a dosimetrist under the supervision of the physicist, uses special computer software to devise a treatment plan; he or she calculates the exposures and beam configuration to conformally treat the target(s) to the prescribed dose.
A highly trained radiation therapist positions the patient on the treatment table and operates the machine from an adjacent protected area. The radiation therapist can observe the patient through a window or on a closed-circuit television and is able to communicate with the patient throughout the procedure. In the case of the Gamma Knife, the neurosurgeon and/or radiation oncologist may help position the patient for treatment and the radiation oncologist may operate the machine.
The radiation therapy nurse assesses the patient, provides the patient with information about the treatment, monitors the patient during treatment, and helps answer questions after treatment.
A neurologist or neuro-oncologist may participate with the radiation oncologist and neurosurgeon in the multidisciplinary team that considers various treatment options for individual cases and helps decide who may benefit from radiosurgery for lesions in the brain.
What equipment is used?
-
There are three basic kinds of equipment, each of which uses different instruments and sources of radiation:
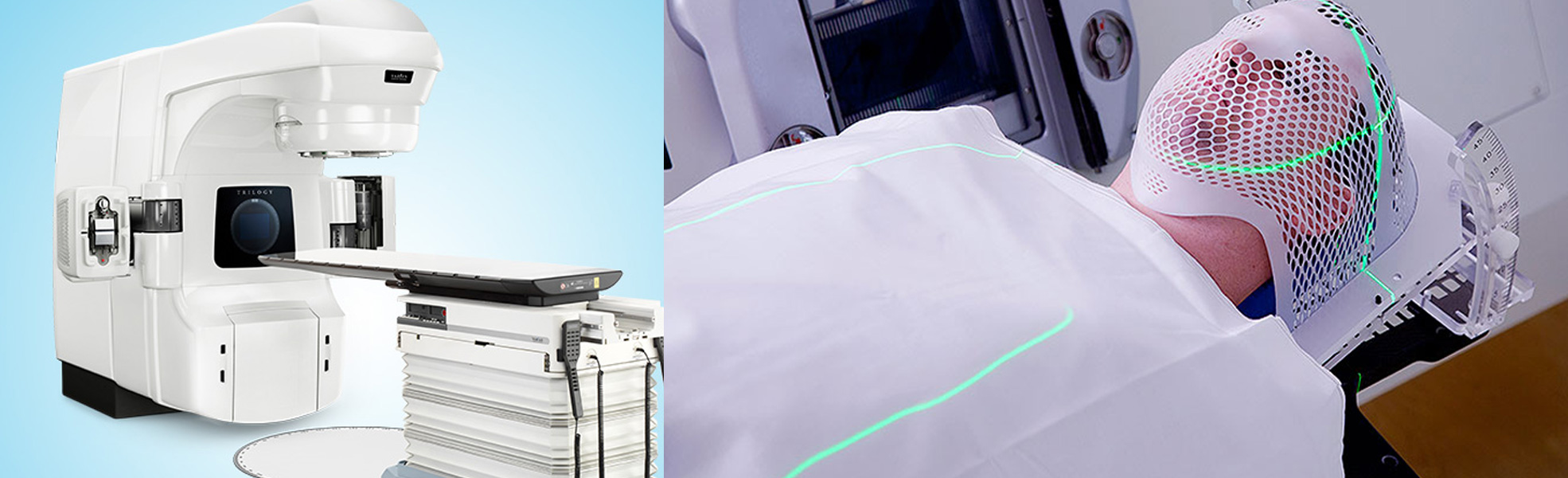
Linear accelerator (LINAC) machines, prevalent throughout the world, deliver high-energy x-rays, also known as photons. The linear accelerator can perform SRS on larger tumors in a single session or during multiple sessions, which is called fractionated stereotactic radiotherapy.
Proton beam or heavy-charged-particle radiosurgery is in limited use in North America, though the number of centers offering proton therapy has increased dramatically in the last several years. See the Proton Therapy page for more information.

The equipment is operated by a radiation therapist, a highly trained technologist. The overall treatment plan is created and supervised by the radiation oncologist, a highly trained physician specializing in treating cancer with radiotherapy.
How is the procedure performed?
• Stereotactic Radiosurgery Using the Gamma Knife Gamma Knife radiosurgery involves four phases: placement of the head frame, imaging of the tumor location, computerized dose planning, and radiation delivery. In the first phase, a nurse will place a small needle in your hand or arm to give you medications and contrast, if needed, for imaging. A neurosurgeon will use local anesthesia to numb two spots on your forehead and two spots on the back of your head. A box-shaped head frame will be attached to your skull using specially designed pins to keep your head from moving within the frame until the treatment session is finished. This lightweight aluminum head frame is also a guiding device that makes sure the Gamma Knife beams are focused exactly where the treatment is needed. Next, you will be taken to an imaging area where a magnetic resonance imaging (MRI) scan will be performed to show the exact location of the tumor in relation to the head frame. In some cases, a computed tomography (CT) scan may be performed instead of, or in addition to, an MRI scan. If you are having treatment for an arteriovenous malformation, you may also have an angiogram. New developments in Gamma Knife software allow for pre-planning. Therefore, you may have your treatment planning MR images prior to the day of your treatment to improve the efficiency of the treatment process. During the next phase, you will be able to relax for an hour or two while your treatment team identifies the tumor(s) for treatment and develops a treatment plan using special computer software to optimally irradiate the tumor and minimize dose to surrounding normal tissues. Next, you will lie down on the Gamma Knife bed and your head frame will be fixed to the machine before beginning treatment. You will be made comfortable with a pillow or wedge-shaped sponge under your knees and a blanket over you. The treatment team will then go to the control area outside the treatment room to begin your treatment. You will be able to talk to your physician through a microphone in the helmet, and a camera will allow the team to see you at all times. The bed you are lying on will move backward into the Gamma Knife machine. You will not feel the treatment and the machine is very quiet. Depending on the Gamma Knife model and the treatment plan, the whole treatment may be performed without interruption or it may be broken up into multiple smaller parts. The total treatment may last less than one hour or up to four hours. A chime will sound when the treatment is complete and the bed will return to its original position. As soon as the treatment is finished, you will sit up and the head frame will be removed. In most cases, you should be able to go home soon afterward. • Radiosurgery Using the Linear Accelerator Linear accelerator (LINAC) SRS is similar to the Gamma Knife procedure and its four phases: head frame placement, imaging, computerized dose planning and radiation delivery. LINAC technology is much more common than Gamma Knife technology and has been in practice for a similar length of time. Unlike the Gamma Knife, which remains motionless during the procedure, part of the LINAC machine (called a gantry) rotates around the patient delivering the radiation beams from different angles. Obtaining the MRI before frame placement is also a more routine pre-planning practice with LINAC-based SRS. A CT with the frame in place is also commonly acquired. a robotic arm moves the compact LINAC around the patient under image-guidance.