Prostate Cancer treatment in Delhi, Prostate Cancer Treatment in India
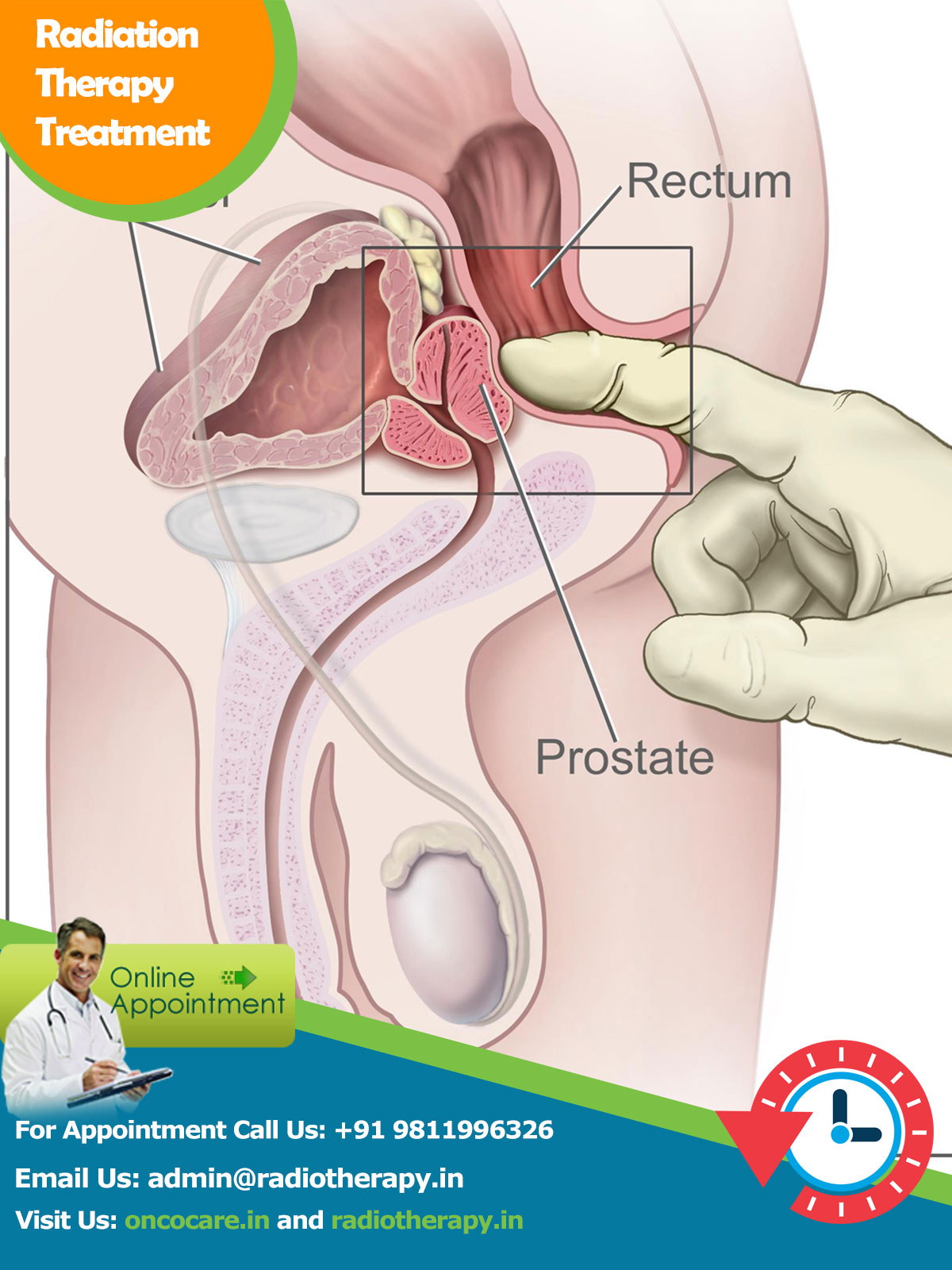
Prostate Cancer forms an important part of male reproductive system. Prostate Cancer is located just beneath the bladder encircling the urethra at its origin.
The main function of the prostate cancer is to store and secrete a clear, slightly alkaline fluid that constitutes 10-30% of the volume of the seminal fluid that, and along with spermatozoa, constitutes semen. The rest of the seminal fluid is produced by the two seminal vesicles. The alkalinity of seminal fluid helps neutralize the acidity of the vaginal tract, prolonging the lifespan of sperm.
Prostate Cancer is anatomically divided into 5 lobes – Anterior, Median, Posterior and two lateral lobes.
Histologically, it is divided into 3 lobes
Peripheral zone (PZ) :
Composes up to 70% of the normal prostate gland in young men. It is from this portion of the gland that more than 70% of prostatic cancers originate.
Central zone (CZ) :
Constitutes approximately 25% of the normal prostate gland. The central zone accounts for roughly 2.5% of prostate cancers although these cancers tend to be more aggressive.
Transition zone (TZ):
Responsible for 5% of the prostate volume at puberty. The transition zone surrounds the proximal urethra and is the region of the prostate gland which grows throughout life and is responsible for the disease of benign prostatic enlargement (BPH).
Incidence of prostate cancer in US is 190/100,000 men. It forms about 33% of all non skin cancers in US. Highest incidence rates have been seen in Scandinavia and lowest in Asia. African Americans have higher incidence and mortality rate in US.
According to the Indian National Cancer registry report of 2001-2004 prostate cancer rank among the five most common cancers in Delhi, Mumbai and Bangalore registries. Incidence has increased primarily because of two reasons.
1. Increased life expectancy: Median age of diagnosis is 68 yrs. Incidence increases sharply after 65 yrs. According to the autopsy data 70% of men older than 80 yrs of age and 40% men more than 50 yrs have pathological evidence of disease.
2. Increased prostate cancer screening owing to increased awareness.
Investigations
-
1.Patients with localized prostatic carcinoma are frequently asymptomatic; the diagnosis is often made with a screening PSA test.
2.Patients with locally advanced tumors have presented with bladder outlet obstructive symptoms such as urinary hesitancy, decreased force of the urinary stream, and post void dribbling s the tumor impinges on the membranous urethra. 3.Chronic obstruction and bladder distention can lead to decreased compliance of the detrusor muscle that is manifested by symptoms of urinary frequency, urgency, and nocturia (increased urination at night). 4.* With local invasion into the urethra or ejaculatory ducts, patients may experiencehematuria (blood in urine) or hematospermia(blood in semen). 5.* As the disease penetrates the capsule of the prostate, there may be invasion into the neurovascular bundles that course along the lateral aspects of the prostate, leading to erectile dysfunction. 6.* Disseminated disease frequently manifests as Bone pain from distant osseous metastases.
Diagnostic Work-Up

Routine
1.Clinical history and clinical examination 2.Digital rectal examination 3.Laboratory Complete blood cell count, blood chemistry profile 4.Serum PSA (total, free, percentage free) 5.Plasma acid phosphatases (prostatic/total) 6. Radiographic imaging Magnetic resonance imaging ( MRI )with endorectal coil 7.Radioisotope bone scan (PSA >20) 8.Computed tomography ( CT )of pelvis 9.Chest radiograph (Chest X-Ray )(in patients with high risk for metastatic disease) 10.Transrectal ultrasonography (for biopsy guidance) 11.Needle biopsy of prostate (transrectal, transperineal): A 6 quadrant and nowadays preferably a 8 quadrant biopsy is advisable 12.Staging lymph node dissection (high risk for lymph node metastases) Transrectal Ultrasonography: TRUS is used routinely for guidance during the transrectal biopsy and during prostate brachytherapy. However, only prostate cancers located in the peripheral zone can be reliably detected by ultrasonography. Computed Tomography (CT Scan): The primary role of CT in prostate cancer is to determine the size of the gland, radiation therapy treatment planning, and assessment of pelvic nodal metastases. It is however difficult to detect any capsular extension, or seminal vesicle involvement. Magnetic resonance imaging (MRI): Soft tissues are clearly identified using MRI. Currently, the best imaging study for prostate cancer is endorectal MRI. Both T1- and T2-weighted images are taken. T1 images can detect blood in the prostate, whereas T2 images help define the internal architecture of the prostate and seminal vesicles including any suspicious lesion. Any extracapsular extension (ECE) and seminal vesicle invasion (SVI), or invasion of the neurovascular bundles (NVBs) can be better picked up using MR Spectroscopy used along with MRI Bone Scan: A bone scan detects for any distant site of bony involvement. Chances of having a positive bone scan are seen in patients with high PSA (>20 ng/ml).Treatment
-
Management of cesophageal cancer can be surgery if in early operable stage or a combination of radiotherapy and chemotherapy known as concurrent chemo radiotherapy. Surgery involves excision of the tumor along with some healthy tissue margin & reconstruction of esophagus to permit oral food intake. Different techniques of surgeries are used for different tumor locations. Post operative or pre operative chemotherapy and radiotherapy may be required in certain conditions.
With advancement in technology, the role of radiotherapy has emerged greatly. Radiotherapy & chemotherapy used together gives results comparable to surgery with preservation of organ. Patient who are medically unfit for surgery or who desires organ preservation can be treated by chemo-radiotherapy with similar tumor control & survival rate as achieved by surgery.
Role of Radiotherapy
Radiotherapy, is a primary treatment modality in the treatment of Carcinoma Oesophagus. In the past radiotherapy has not been used upto optimal doses required to treat cancer, because of the limitation of the dose to surrounding vital organs like lungs, heart, spinal cord etc. With the advent of newer & precise techniques of radiotherapy planning & delivery such as 3D Conformal radiotherapy & Intensity Modulated Radiotherapy, optimal tumoricidal doses can be delivered without crossing the tolerance limit of surrounding critical structures.
Procedure of Radiotherapy Treatment

The process of radiotherapy treatment starts with the making of customized plastic orfit cast (perforated thermo-plastic sheet) of chest. This cast is tailor made for each patient & serve the purpose of preventing any movement at the time of radiation treatment. It also spares the patient from having tatto marks on skin required for daily field alignment. A Planning CT scaan of the chest is done with the orfit cast on the patient and is used for radiation treatment planning. The radiation oncologist then marks the tumor and other normal organs on the treatment planning system. A physicist team then makes the desired plan and the oncologist selects the best plan and approves it for the treatment of patient clinically. In our hospital the radiation treatment is usually given for 25 fractions (5 days / week from Monday to Friday). The treatment time every day ranges between 15 – 25 minutes. The radiation is given in 2-3 phases,initially the dose is delivered to entire disease involved part with generous margins. Later in step wise manner the radiation field is shrinked to delivered higher doses to tumor involved part with smaller margins. Once radiation is complete it is followed by 2 fractions of boost radiotherapy by Intraluminal technique. In this procedure, under local anesthesia a hollow tube is inserted in the oesophagus. This tube is connected to radiation source and tumor can be treated with the remaining dose (usually 2 fractions of Intraluminal Brachytherapy). The common side effects of Radiotherapy,are generalized weakness, loss of appetite and mild burning on swallowing. But these side effects are mild and are easily manageable. Different institution follows different chemotherapy schedules along with Radiotherapy, to enhance the effect of radiation.Most commonly used protocol are infusion of combination chemotherapy starting from D1- D5 of radiotherapy (cycle – 1) followed by similar cycles at interval of 3-4 weeks. Adding chemotherapy to radiation improves result in terms of disease control and better survival rate.